Moderate COPD with Subsequent Bronchospasm
Description
A 62 year-old patient developed pneumonia while working on a water purification system. He has 90- pack year history of cigarette smoking (2 packs per day x 45 years), has type II diabetes and primary hypertension managed with oral medications. He uses a rescue inhaler (albuterol) and is on a maintenance inhaled corticosteroid. His pre-deployment FEV-1 is 43% of predicted. The patient is 5'9" tall, weighs 210 lbs and has no known allergies.
Chest radiograph demonstrates left-lower lobe consolidation, haziness in the right lower lobe, flattened diaphragms and hyperinflation in the upper lung fields. Heart rate is normal sinus rhythm and occasional PVC's. Patient is sedated and not triggering ventilator.
Segment Validation
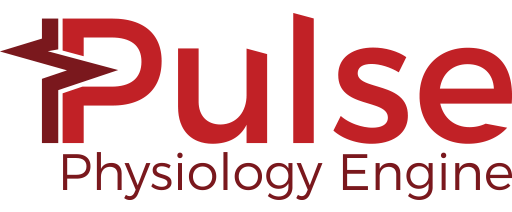
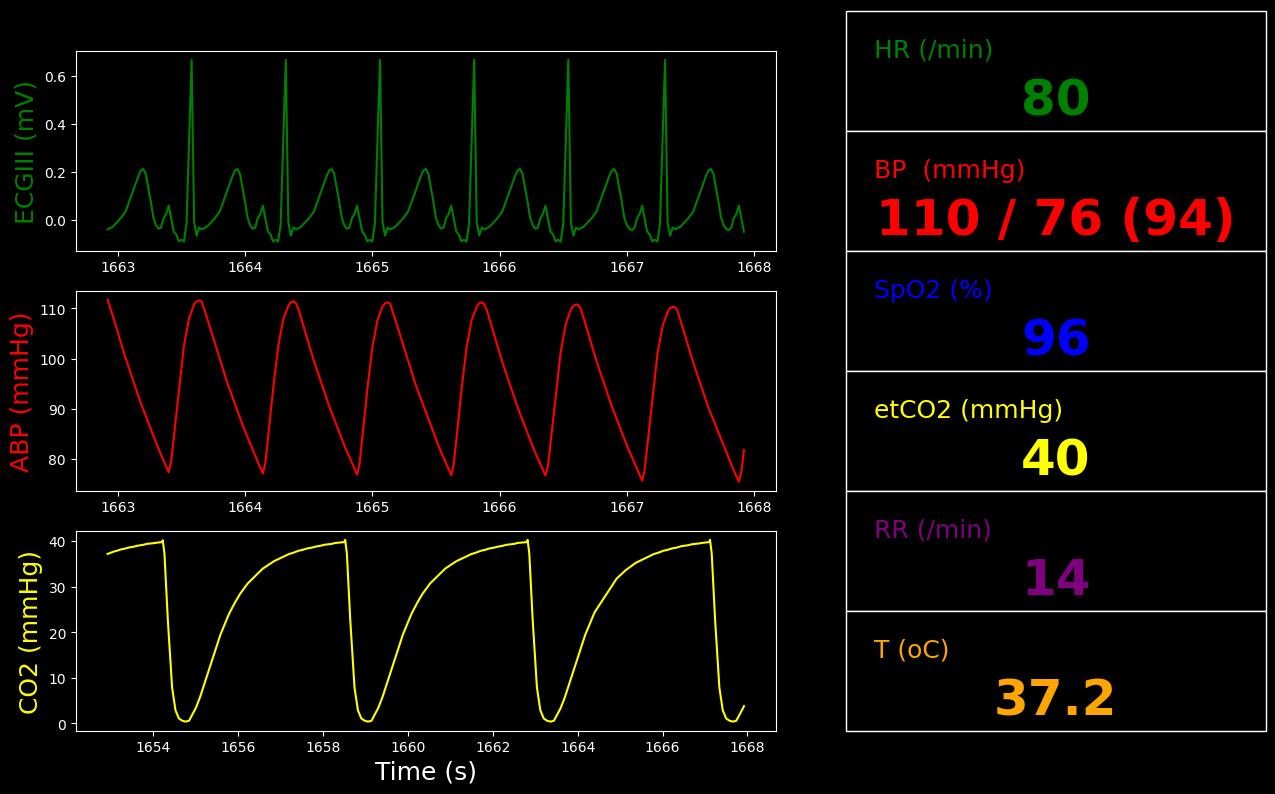
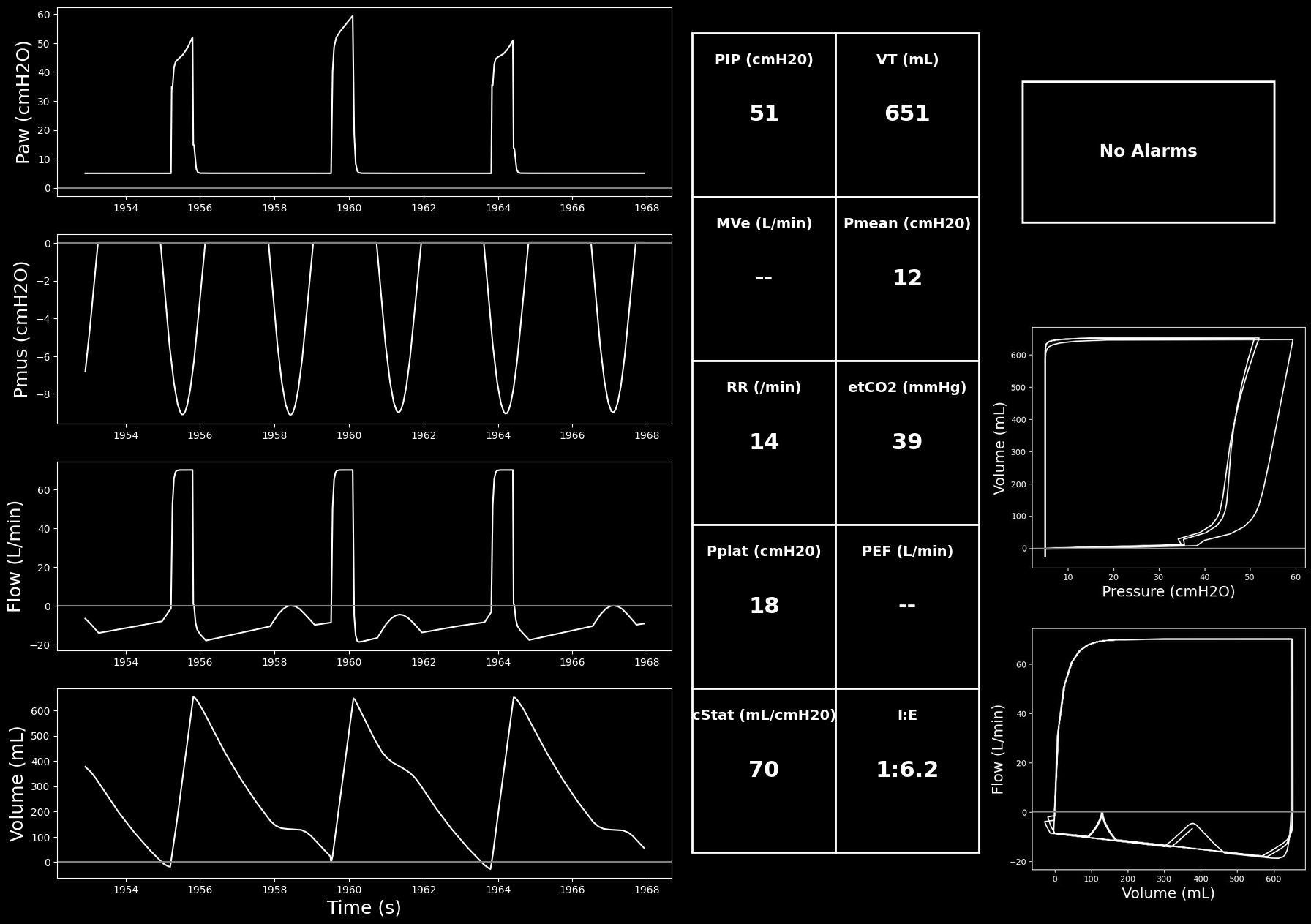
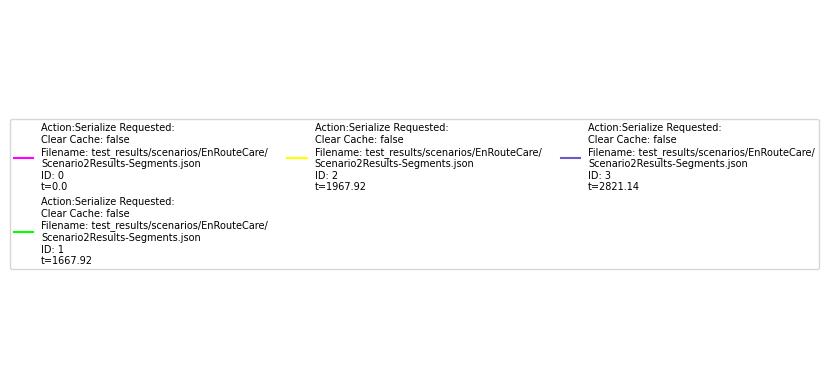
Segment 1
Learning Objectives:
- Assess baseline status
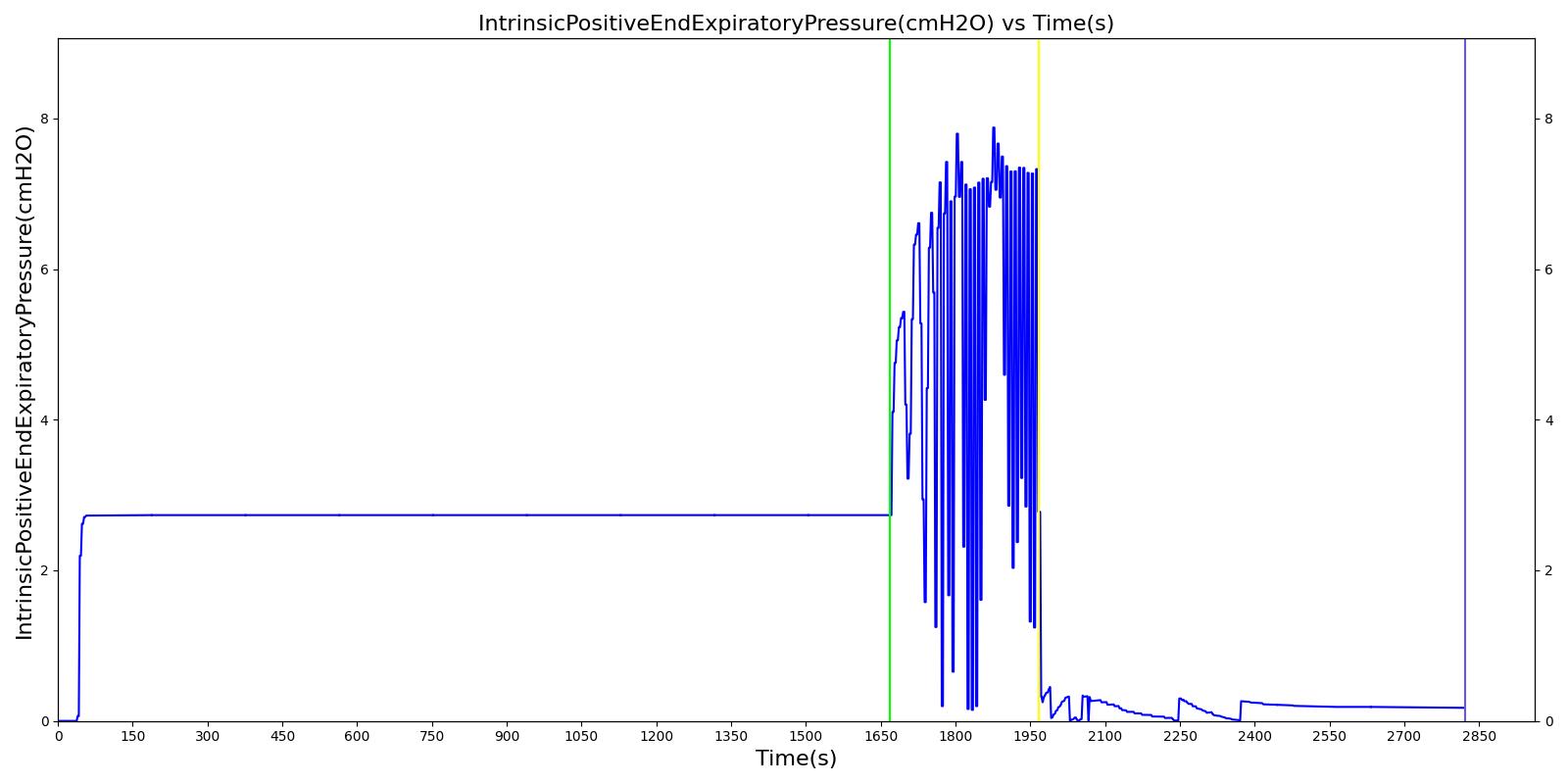
- Recognize presence of autoPEEP (from flow waveform)
- Suspect obstructive lung disease (high minute ventilation requirement but high SpO2 and low Pplat)
Recommended Actions:
- None
Ventilator settings are:
| Mode | VT (L) | PIP (cmH2O) | Flow (L/min) | I:E | TI (s) | RR (bpm) | PEEP (cmH2O) | FiO2 |
|---|---|---|---|---|---|---|---|---|
| VC-AC | 0.650 | NA | 70 | NA | 0.6 | 14 | 5 | 0.4 |
Ventilator alarm settings are:
- High PIP = 50 cmH2O (~10 cmH2O above the initial value or a max of 50 cmH2O)
- Low MVe = 6.8 L/min (~25% below the initial value)
- Low VT = 490 mL (~25% below the initial value)
- High RR = 24 bpm (~10 bpm above the initial value or a max of 40 bpm)
| Property Name | Validation | Engine Value | Percent Error | Percent Change | Notes |
|---|---|---|---|---|---|
| MechanicalVentilator-TidalVolume(mL) | EqualTo 650 | 650 | 0.0590% | VT (measured) | |
| InspiratoryRespiratoryResistance(cmH2O_s/L) | EqualTo 24 [381] [270] | 24.0 | 0.196% | Rinsp for moderate COPD | |
| ExpiratoryRespiratoryResistance(cmH2O_s/L) | EqualTo 36 [381] | 36.9 | 2.45% | Rexp for moderate COPD | |
| RespiratoryCompliance(mL/cmH2O) | EqualTo 68 [229] | 64.5 | 5.22% | C for moderate COPD | |
| PhysiologicDeadSpaceTidalVolumeRatio | EqualTo 0.49 [113] | 0.477 | 2.59% | VD/VT for moderate COPD | |
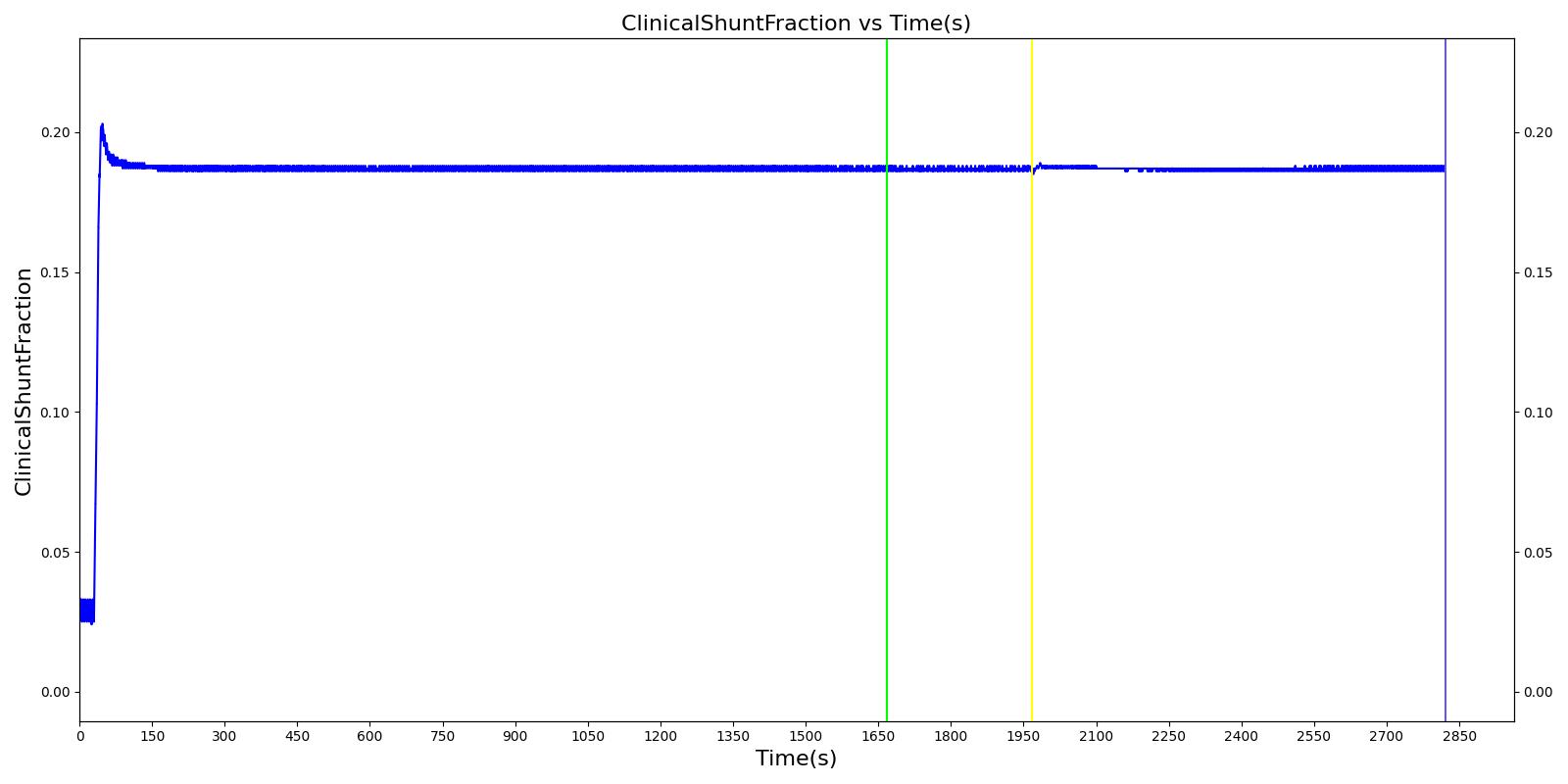
| ClinicalShuntFraction | EqualTo 0.19 [364] | 0.187 | 1.79% | QS/QT for moderate COPD (determined from blood gas values) |
| Property Name | Engine Value |
|---|---|
| Patient-Height(in) | 69.0 |
| Patient-IdealBodyWeight(kg) | 70.7 |
| InspiratoryRespiratoryResistance(cmH2O_s/L) | 24.0 |
| ExpiratoryRespiratoryResistance(cmH2O_s/L) | 36.9 |
| RespiratoryCompliance(mL/cmH2O) | 64.5 |
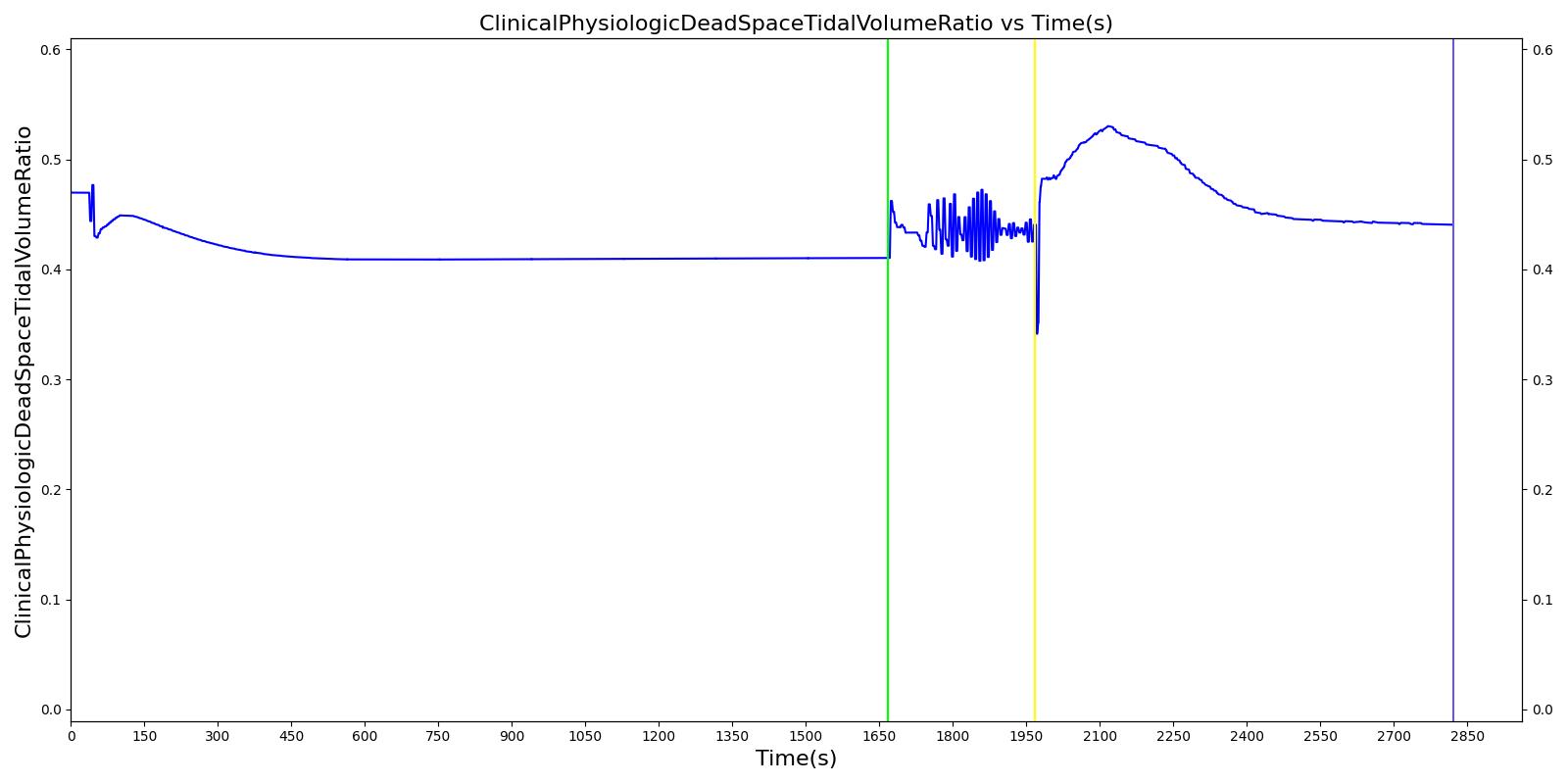
| ClinicalPhysiologicDeadSpaceTidalVolumeRatio | 0.410 |
| ClinicalShuntFraction | 0.187 |
| MechanicalVentilator-TidalVolume(L) | 0.650 |
| BloodPH | 7.37 |
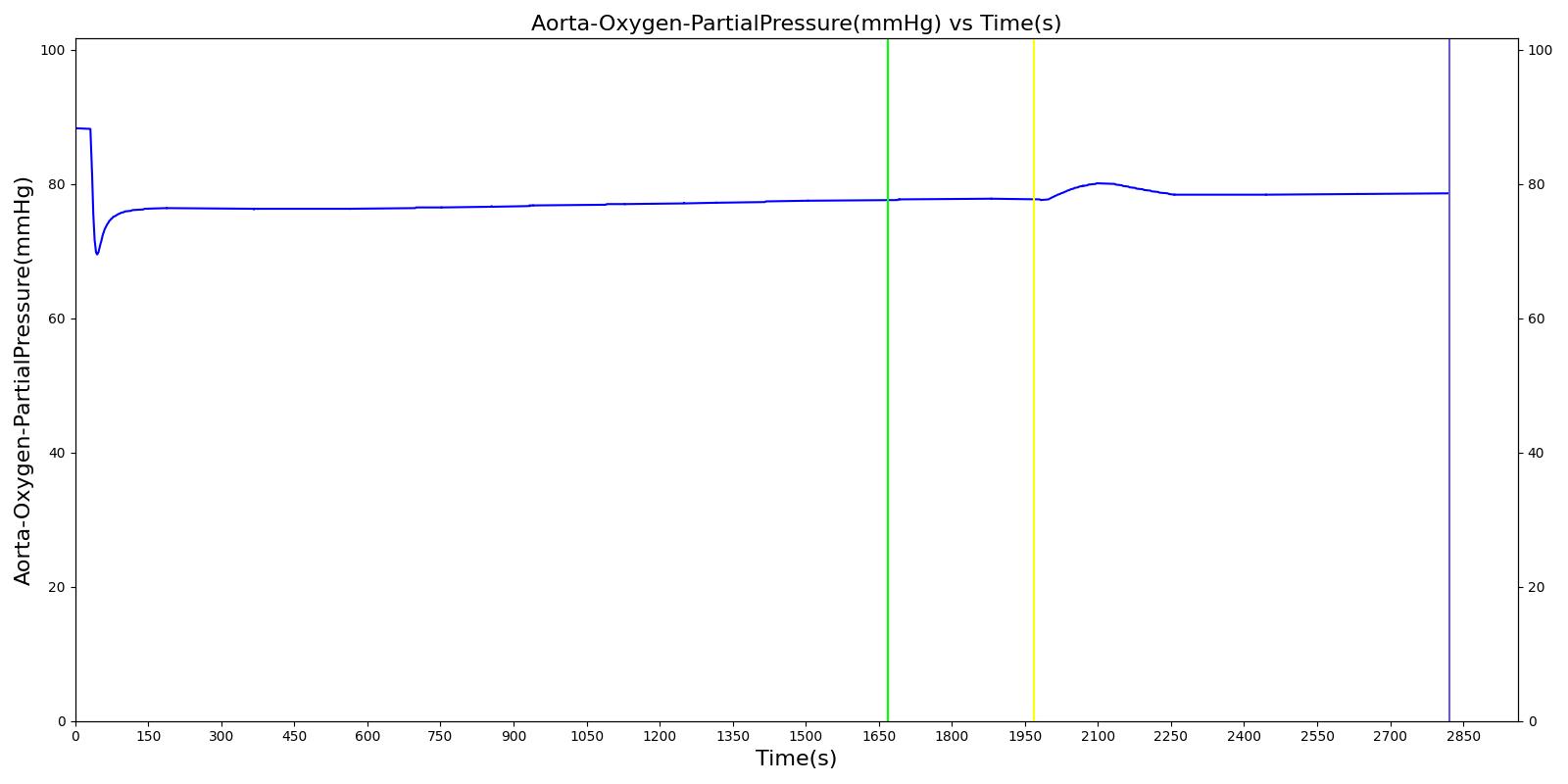
| Aorta-Oxygen-PartialPressure(mmHg) | 77.6 |
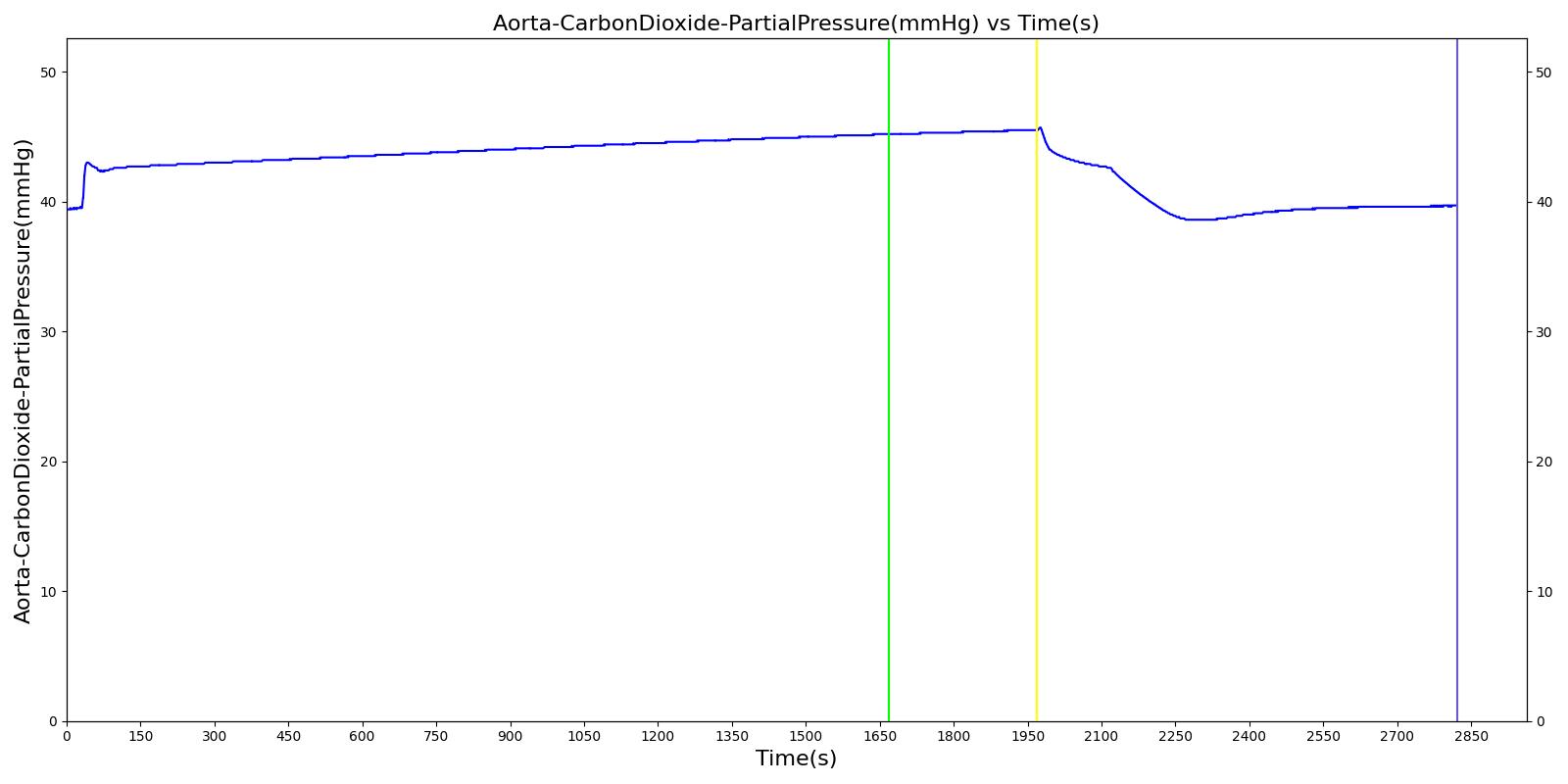
| Aorta-CarbonDioxide-PartialPressure(mmHg) | 45.2 |
| Aorta-Bicarbonate-Molarity(mEq/L) | 26.1 |
| OxygenSaturation | 0.956 |
| HorowitzIndex(mmHg) | 194 |
| IntrinsicPositiveEndExpiratoryPressure(cmH2O) | 2.73 |
| MechanicalVentilator-RespirationRate(1/min) | 14.0 |
| MechanicalVentilator-MeanAirwayPressure(cmH2O) | 9.82 |
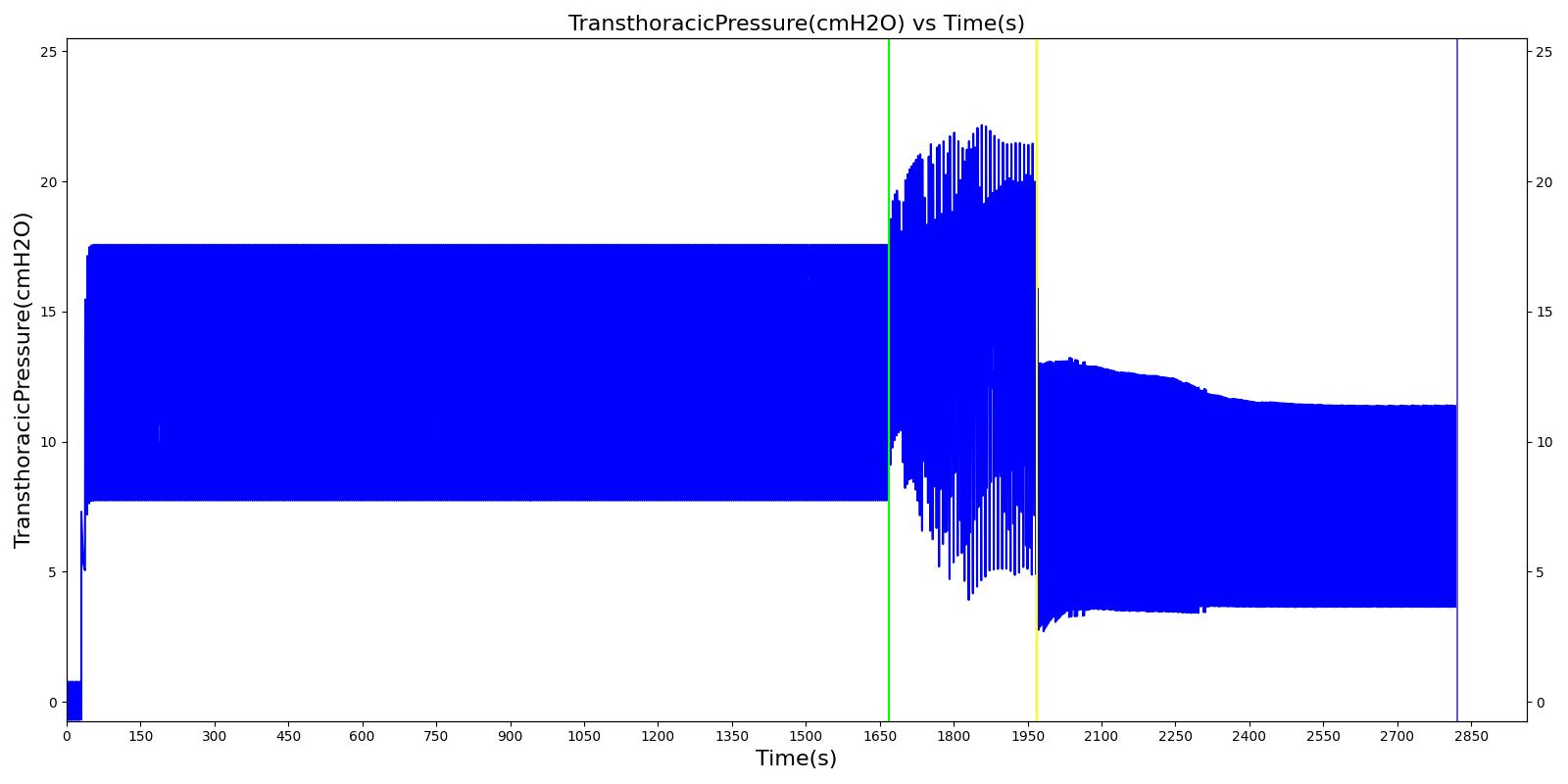
| MechanicalVentilator-PeakInspiratoryPressure(cmH2O) | 45.0 |
| MechanicalVentilator-PlateauPressure(cmH2O) | 17.3 |
| HeartRate(1/min) | 79.9 |
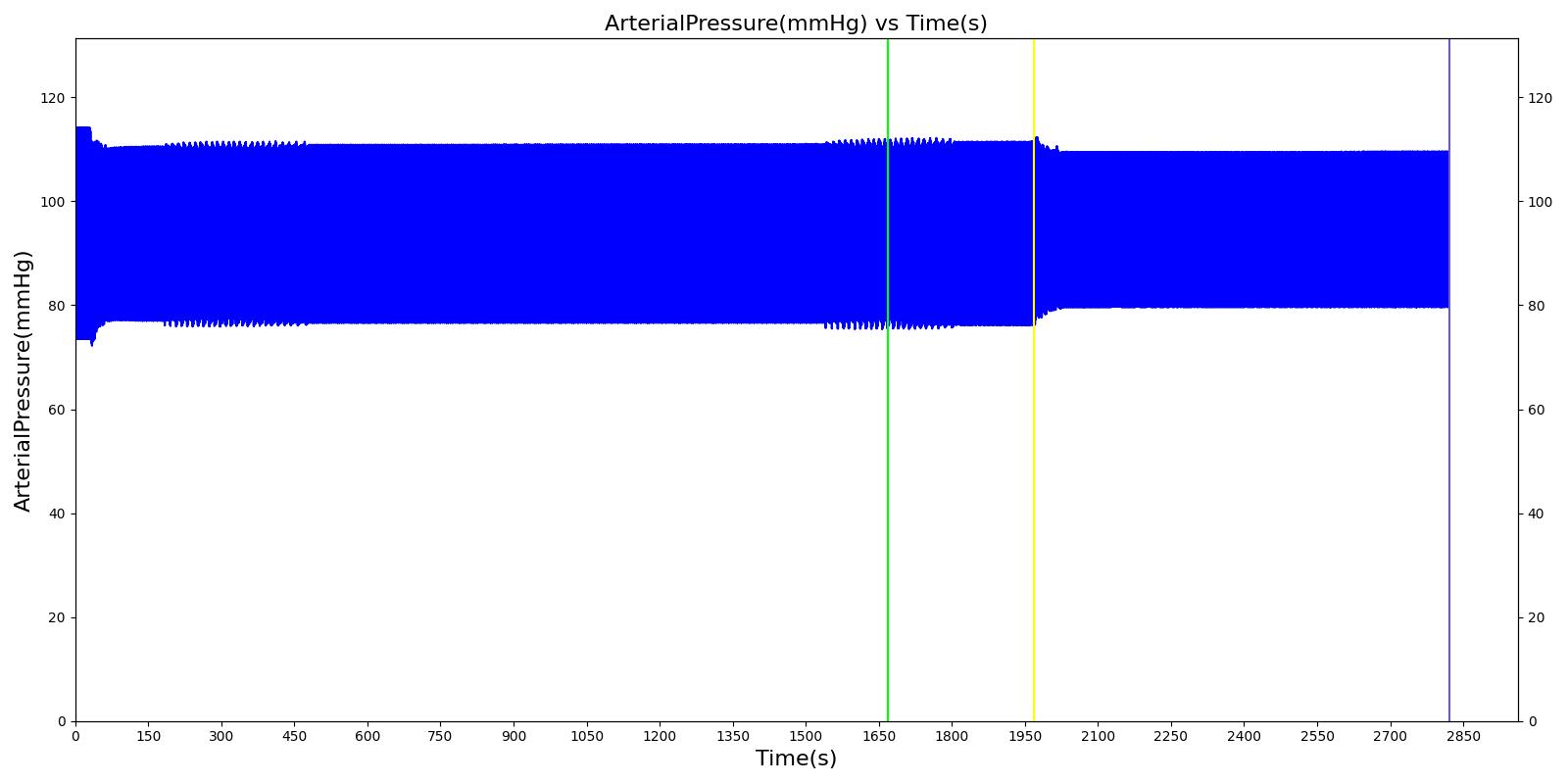
| SystolicArterialPressure(mmHg) | 110 |
| DiastolicArterialPressure(mmHg) | 75.7 |
| MechanicalVentilator-TotalPulmonaryVentilation(L/min) | 9.08 |
| MechanicalVentilator-InspiratoryResistance(cmH2O_s/L) | 24.0 |
| MechanicalVentilator-ExpiratoryResistance(cmH2O_s/L) | 37.0 |
| MechanicalVentilator-StaticRespiratoryCompliance(mL/cmH2O) | 63.9 |
| MechanicalVentilator-DynamicRespiratoryCompliance(mL/cmH2O) | 16.2 |
| MechanicalVentilator-EndTidalCarbonDioxidePressure(mmHg) | 38.3 |
| MechanicalVentilator-EndTidalOxygenPressure(mmHg) | 261 |
| MechanicalVentilator-ExpiratoryTidalVolume(L) | 0.650 |
| MechanicalVentilator-InspiratoryExpiratoryRatio | 0.162 |
| MechanicalVentilator-InspiratoryTidalVolume(L) | 0.650 |
| MechanicalVentilator-PeakExpiratoryFlow(L/s) | 0.321 |
| MechanicalVentilator-LeakFraction | 0.00 |
| MechanicalVentilator-IntrinsicPositiveEndExpiratoryPressure(cmH2O) | 2.13 |
| MechanicalVentilator-ExtrinsicPositiveEndExpiratoryPressure(cmH2O) | 5.00 |
| MechanicalVentilator-TotalPositiveEndExpiratoryPressure(cmH2O) | 7.13 |
| PhysiologicDeadSpaceTidalVolumeRatio | 0.477 |
| PhysiologicShuntFraction | 0.193 |
| TotalRespiratoryModelInspiratoryResistance(cmH2O_s/L) | 23.5 |
| TotalRespiratoryModelExpiratoryResistance(cmH2O_s/L) | 37.0 |
| TotalRespiratoryModelCompliance(mL/cmH2O) | 73.2 |
| ExtrinsicPositiveEndExpiratoryPressure(cmH2O) | 5.01 |
| TotalPositiveEndExpiratoryPressure(cmH2O) | 7.74 |
| EndTidalCarbonDioxidePressure(mmHg) | 40.3 |
| PhysiologicDeadSpace(mL) | 236 |
| AlveolarArterialGradient(mmHg) | 184 |
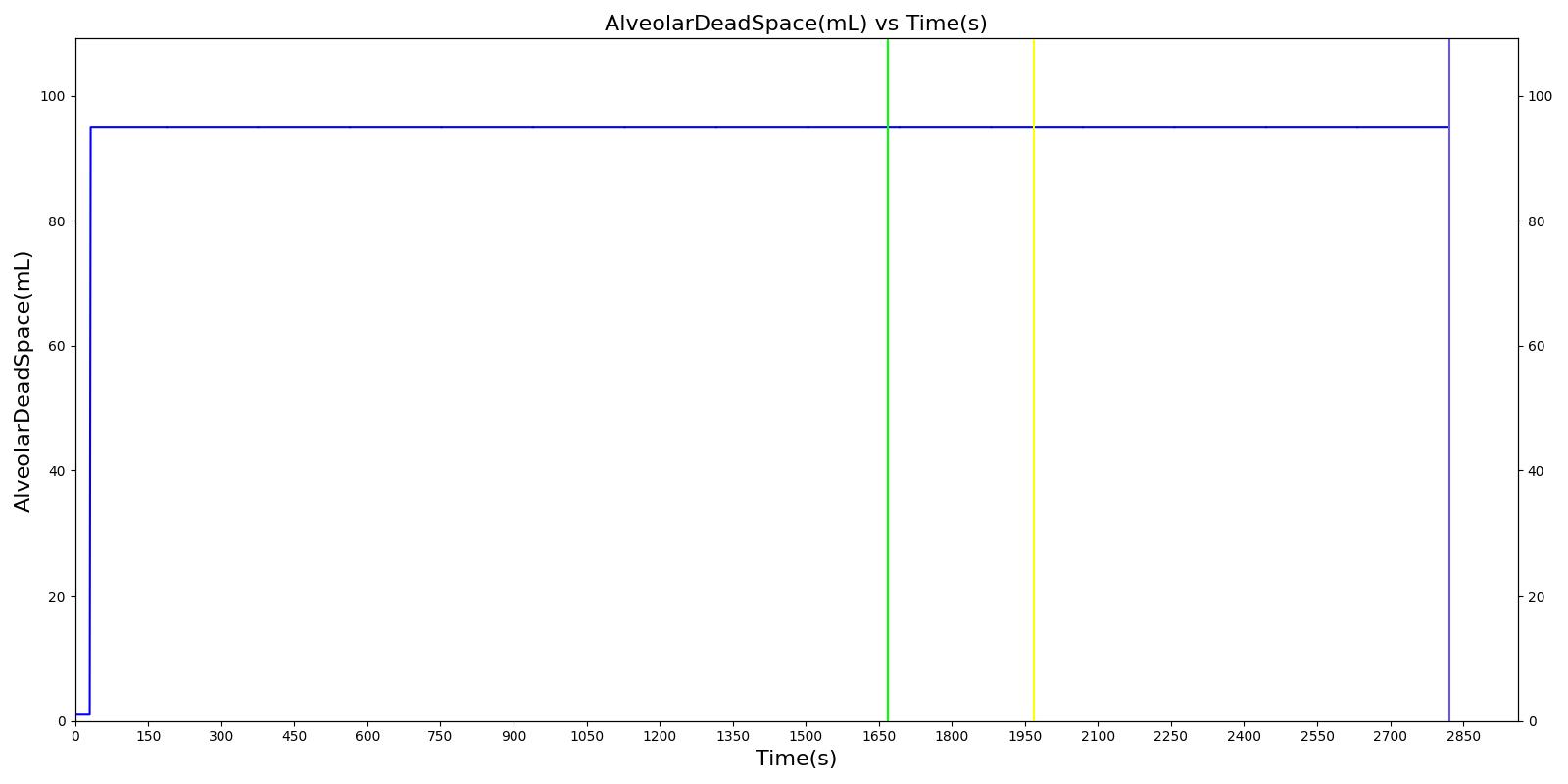
| AlveolarDeadSpace(mL) | 94.9 |
| AnatomicDeadSpace(mL) | 141 |
| ChestWallCompliance(L/cmH2O) | 0.201 |
| FractionOfInspiredOxygen | 0.400 |
| LungCompliance(L/cmH2O) | 0.0972 |
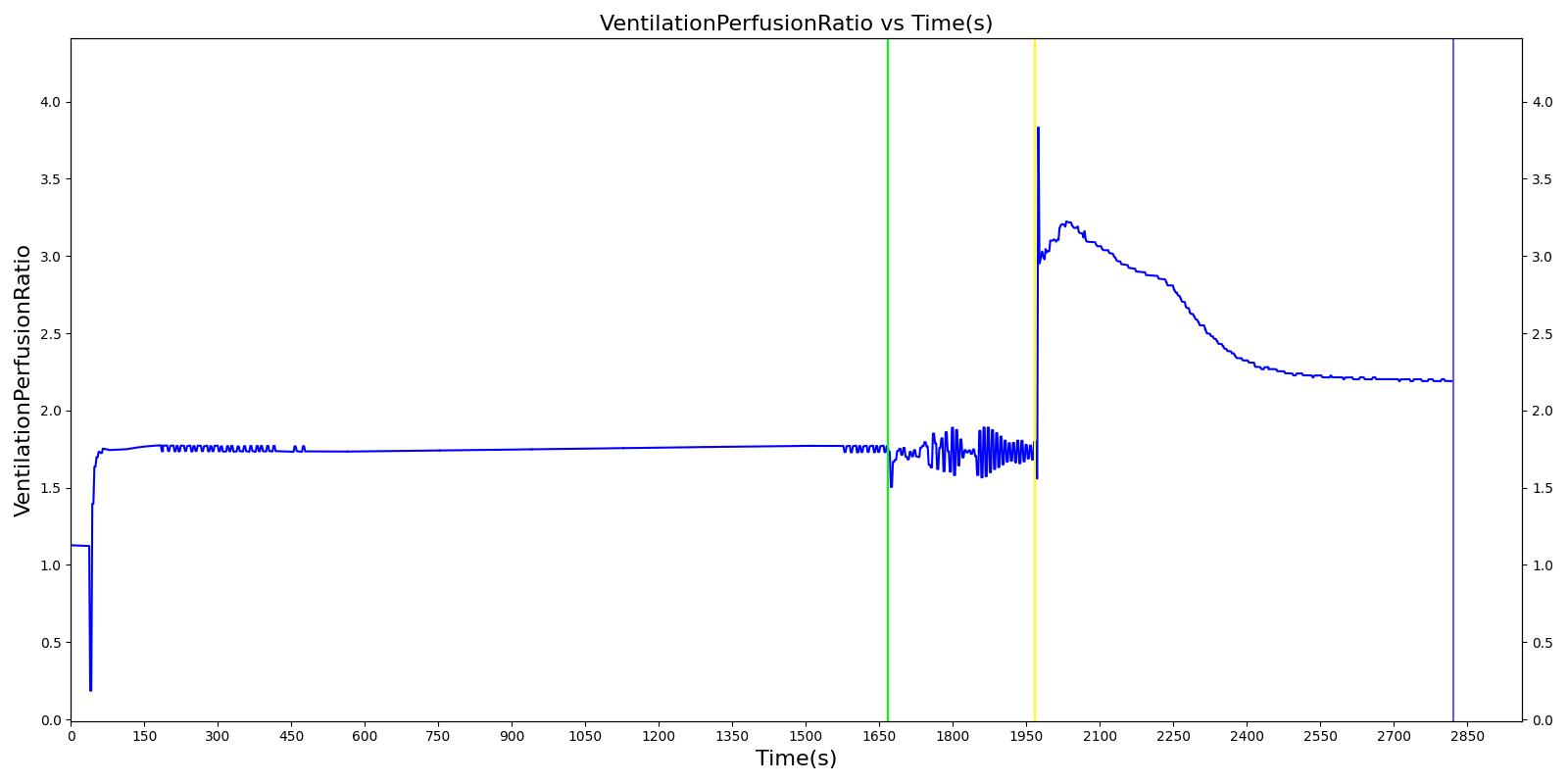
| VentilationPerfusionRatio | 1.73 |
| HeartStrokeVolume(mL) | 68.2 |
| HeartEjectionFraction | 0.519 |
| BloodVolume(L) | 6.61 |
| MeanArterialPressure(mmHg) | 94.1 |
| PulsePressure(mmHg) | 34.6 |
| CardiacOutput(L/min) | 5.45 |
| CarbonDioxideSaturation | 0.173 |
| RespiratoryExchangeRatio | 0.814 |
| SystemicVascularResistance(mmHg_s/mL) | 0.982 |
| OxygenConsumptionRate(mL/min) | 263 |
| CarbonDioxideProductionRate(mL/min) | 214 |
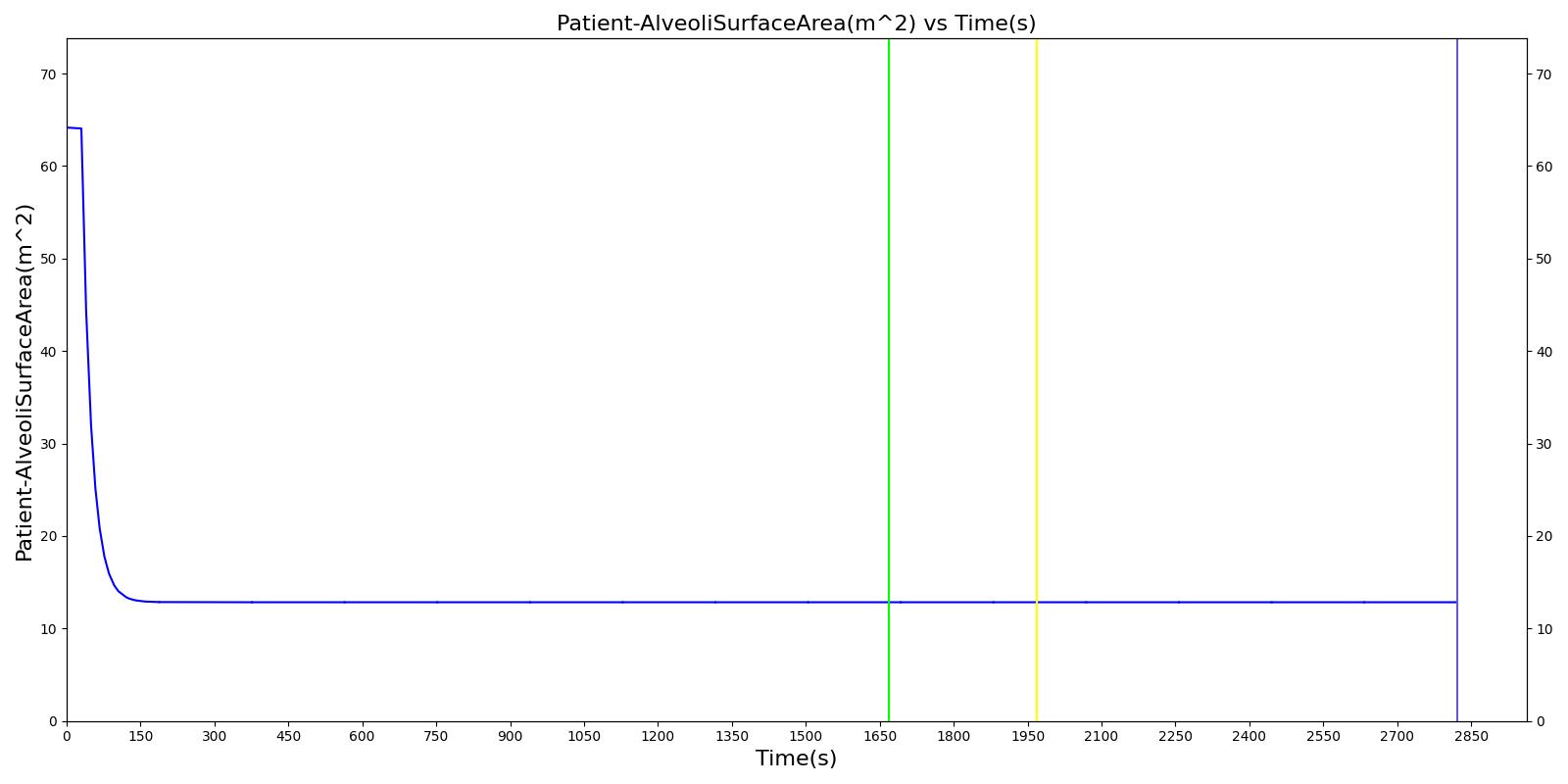
| Patient-AlveoliSurfaceArea(m^2) | 12.8 |
| Patient-ExpiratoryReserveVolume(L) | 0.876 |
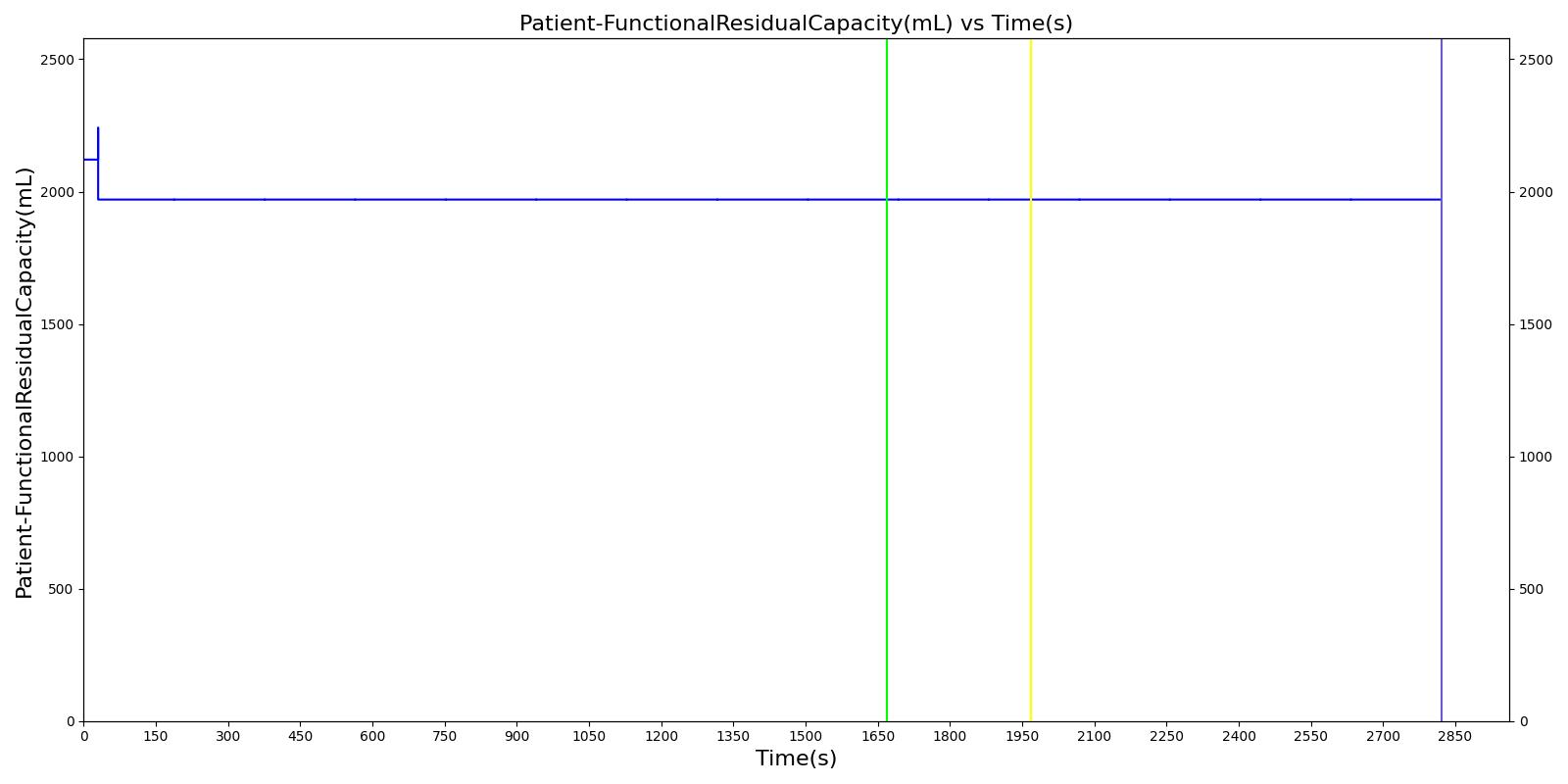
| Patient-FunctionalResidualCapacity(L) | 1.97 |
| Patient-InspiratoryCapacity(L) | 3.13 |
| Patient-InspiratoryReserveVolume(L) | 2.59 |
| Patient-ResidualVolume(L) | 1.09 |
| Patient-TidalVolumeBaseline(L) | 0.540 |
| Patient-TotalLungCapacity(L) | 5.10 |
| Patient-VitalCapacity(L) | 4.00 |
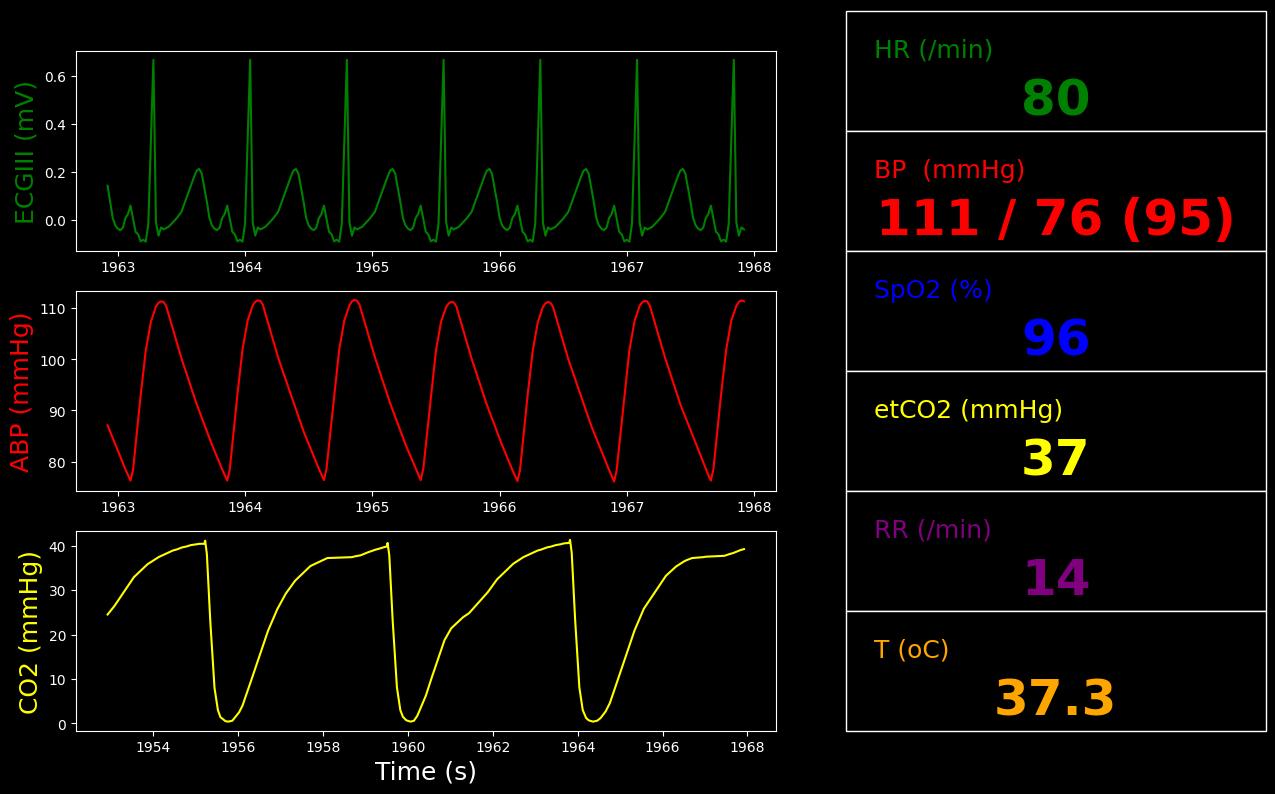
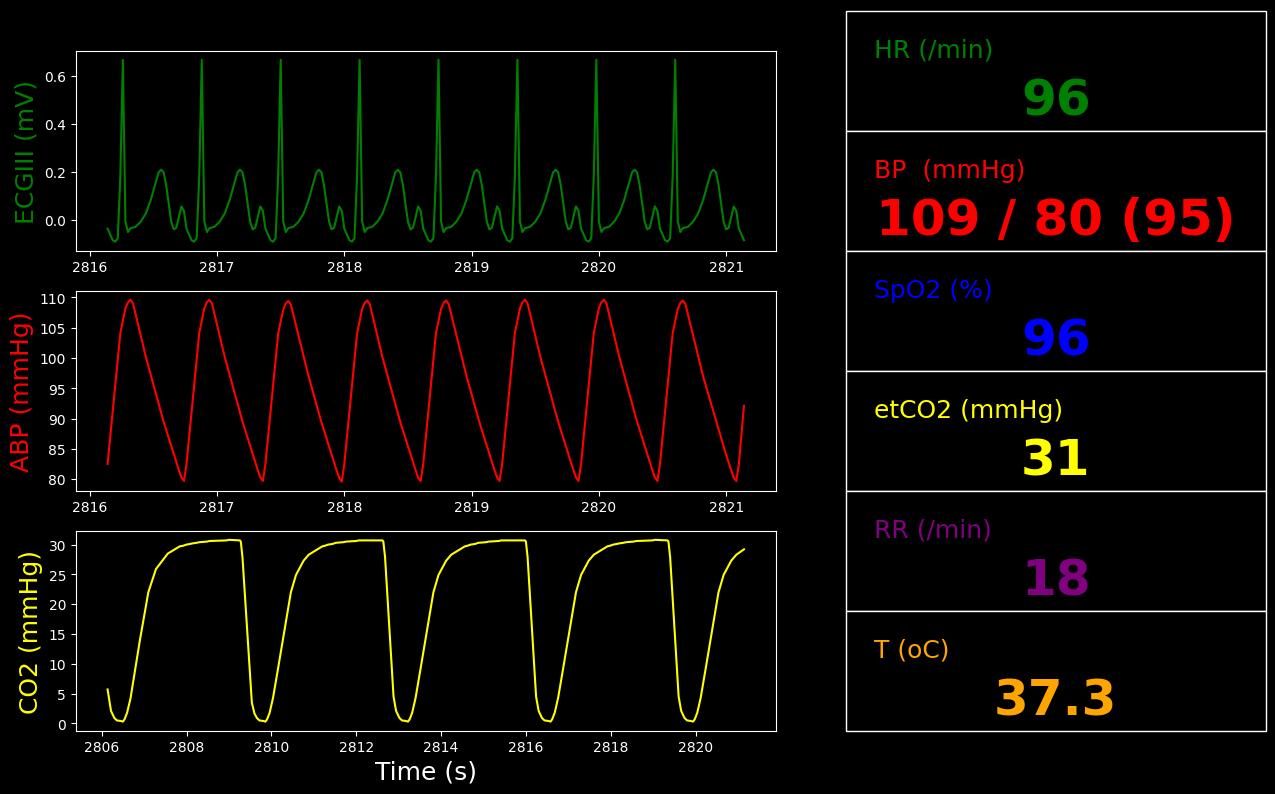
Segment 2
Twenty minutes into the transport the patient is slightly agitated and is making inspiratory efforts that are not in sync with the ventilator.
Learning Objectives:
- Recognize increased airway resistance (PIP much higher than Pplat)
- Recognize autoPEEP (from flow waveform)
- Recognize failed trigger efforts due to autoPEEP (examine expiratory flow waveform)
Recommended Actions:
- Goal shifts to Comfort (improve synchrony) due to failed trigger efforts
- Check airway patency (secretions?) suction ETT
- Check breath sounds (wheezing?) - suspect bronchospasm and consider bronchodilator
| Property Name | Validation | Engine Value | Percent Error | Percent Change | Notes |
|---|---|---|---|---|---|
| MechanicalVentilator-TidalVolume(mL) | LessThan Segment1 (650) | 650 | -0.0685% | VT for PIP alarm cycling | |
| InspiratoryRespiratoryResistance(cmH2O_s/L) | GreaterThan Segment1 (24.0) [304] [308] | 33.3 | 38.9% | Rinsp | |
| ExpiratoryRespiratoryResistance(cmH2O_s/L) | GreaterThan Segment1 (36.9) [304] [308] | 50.6 | 37.0% | Rexp | |
| MechanicalVentilator-PeakInspiratoryPressure(cmH2O) | GreaterThan Segment1 (45.0) [304] [308] | 49.6 | 10.1% | PIP |
| Property Name | Engine Value |
|---|---|
| Patient-Height(in) | 69.0 |
| Patient-IdealBodyWeight(kg) | 70.7 |
| InspiratoryRespiratoryResistance(cmH2O_s/L) | 33.3 |
| ExpiratoryRespiratoryResistance(cmH2O_s/L) | 50.6 |
| RespiratoryCompliance(mL/cmH2O) | 68.5 |
| ClinicalPhysiologicDeadSpaceTidalVolumeRatio | 0.462 |
| ClinicalShuntFraction | 0.188 |
| MechanicalVentilator-TidalVolume(L) | 0.650 |
| BloodPH | 7.33 |
| Aorta-Oxygen-PartialPressure(mmHg) | 77.3 |
| Aorta-CarbonDioxide-PartialPressure(mmHg) | 50.0 |
| Aorta-Bicarbonate-Molarity(mEq/L) | 26.4 |
| OxygenSaturation | 0.951 |
| HorowitzIndex(mmHg) | 193 |
| IntrinsicPositiveEndExpiratoryPressure(cmH2O) | 4.29 |
| MechanicalVentilator-RespirationRate(1/min) | 14.0 |
| MechanicalVentilator-MeanAirwayPressure(cmH2O) | 10.6 |
| MechanicalVentilator-PeakInspiratoryPressure(cmH2O) | 49.6 |
| MechanicalVentilator-PlateauPressure(cmH2O) | 17.7 |
| HeartRate(1/min) | 79.9 |
| SystolicArterialPressure(mmHg) | 111 |
| DiastolicArterialPressure(mmHg) | 76.3 |
| MechanicalVentilator-TotalPulmonaryVentilation(L/min) | 9.07 |
| MechanicalVentilator-InspiratoryResistance(cmH2O_s/L) | 33.1 |
| MechanicalVentilator-ExpiratoryResistance(cmH2O_s/L) | 50.6 |
| MechanicalVentilator-StaticRespiratoryCompliance(mL/cmH2O) | 68.5 |
| MechanicalVentilator-DynamicRespiratoryCompliance(mL/cmH2O) | 14.6 |
| MechanicalVentilator-EndTidalCarbonDioxidePressure(mmHg) | 41.2 |
| MechanicalVentilator-EndTidalOxygenPressure(mmHg) | 248 |
| MechanicalVentilator-ExpiratoryTidalVolume(L) | 0.596 |
| MechanicalVentilator-InspiratoryExpiratoryRatio | 0.162 |
| MechanicalVentilator-InspiratoryTidalVolume(L) | 0.650 |
| MechanicalVentilator-PeakExpiratoryFlow(L/s) | 0.279 |
| MechanicalVentilator-LeakFraction | 0.0825 |
| MechanicalVentilator-IntrinsicPositiveEndExpiratoryPressure(cmH2O) | 3.25 |
| MechanicalVentilator-ExtrinsicPositiveEndExpiratoryPressure(cmH2O) | 5.00 |
| MechanicalVentilator-TotalPositiveEndExpiratoryPressure(cmH2O) | 8.25 |
| PhysiologicDeadSpaceTidalVolumeRatio | 0.477 |
| PhysiologicShuntFraction | 0.193 |
| TotalRespiratoryModelInspiratoryResistance(cmH2O_s/L) | 32.5 |
| TotalRespiratoryModelExpiratoryResistance(cmH2O_s/L) | 50.5 |
| TotalRespiratoryModelCompliance(mL/cmH2O) | 70.6 |
| ExtrinsicPositiveEndExpiratoryPressure(cmH2O) | 5.01 |
| TotalPositiveEndExpiratoryPressure(cmH2O) | 9.30 |
| EndTidalCarbonDioxidePressure(mmHg) | 44.2 |
| PhysiologicDeadSpace(mL) | 236 |
| AlveolarArterialGradient(mmHg) | 163 |
| AlveolarDeadSpace(mL) | 94.9 |
| AnatomicDeadSpace(mL) | 141 |
| ChestWallCompliance(L/cmH2O) | 0.237 |
| FractionOfInspiredOxygen | 0.400 |
| LungCompliance(L/cmH2O) | 0.0971 |
| VentilationPerfusionRatio | 1.42 |
| HeartStrokeVolume(mL) | 68.8 |
| HeartEjectionFraction | 0.520 |
| BloodVolume(L) | 6.62 |
| MeanArterialPressure(mmHg) | 94.9 |
| PulsePressure(mmHg) | 35.0 |
| CardiacOutput(L/min) | 5.50 |
| CarbonDioxideSaturation | 0.341 |
| RespiratoryExchangeRatio | 0.818 |
| SystemicVascularResistance(mmHg_s/mL) | 0.983 |
| OxygenConsumptionRate(mL/min) | 268 |
| CarbonDioxideProductionRate(mL/min) | 219 |
| Patient-AlveoliSurfaceArea(m^2) | 12.8 |
| Patient-ExpiratoryReserveVolume(L) | 0.876 |
| Patient-FunctionalResidualCapacity(L) | 1.97 |
| Patient-InspiratoryCapacity(L) | 3.13 |
| Patient-InspiratoryReserveVolume(L) | 2.59 |
| Patient-ResidualVolume(L) | 1.09 |
| Patient-TidalVolumeBaseline(L) | 0.540 |
| Patient-TotalLungCapacity(L) | 5.10 |
| Patient-VitalCapacity(L) | 4.00 |
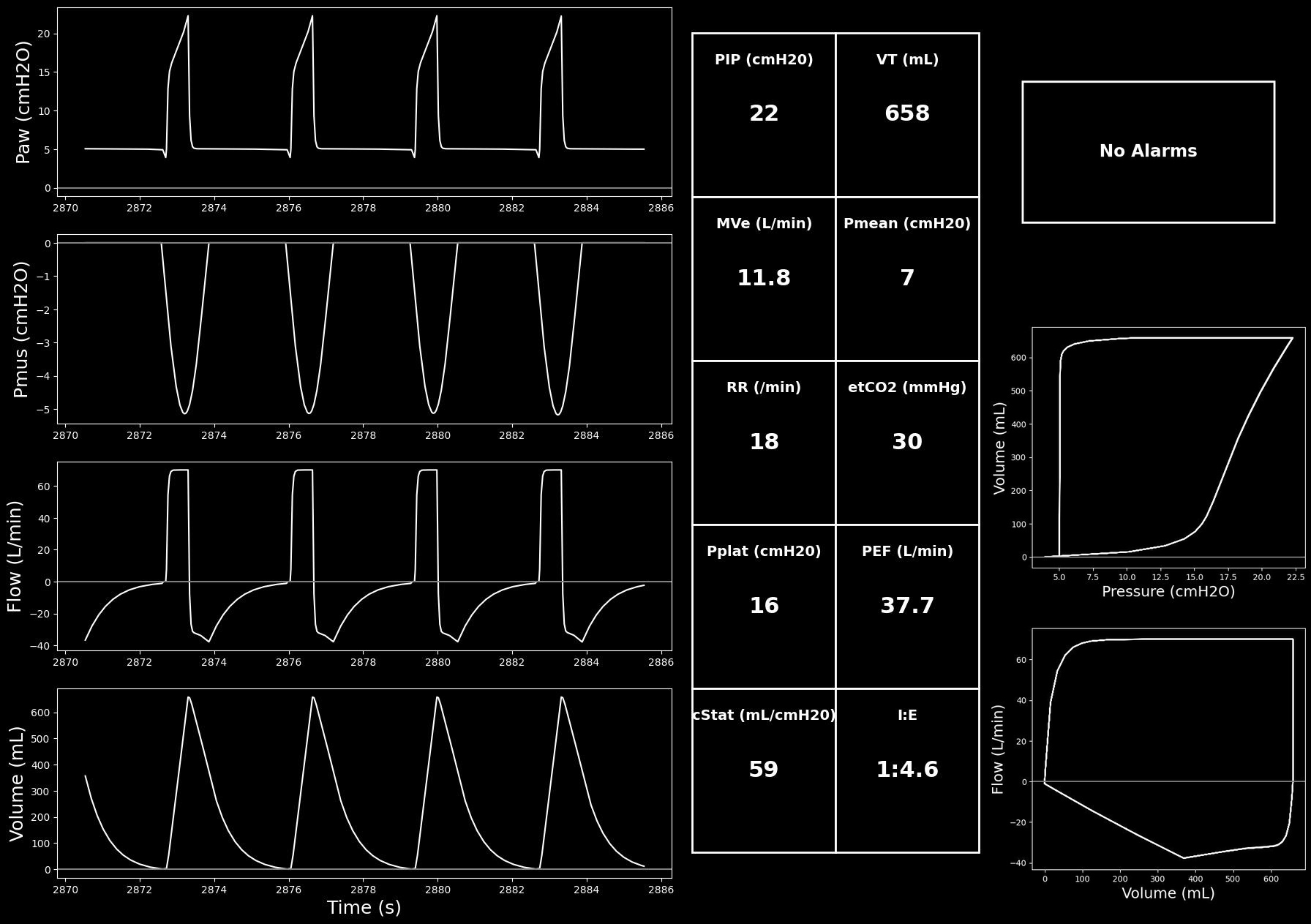
Segment 3
Patient suctioned and albuterol administered.
Learning Objectives:
- Recognize that treatment reduced airway resistance (lower difference PIP - Pplat)
- AutoPEEP reduced
- Failed trigger efforts disappeared
- Recognize that now discordance problem is early cycle
Recommended Actions:
- Goal shifts to Comfort (improve synchrony) due to cycle dyssychrony
- Decrease FiO2
- Consider switching mode to PC-CSV (ie Pressure Support)
| Property Name | Validation | Engine Value | Percent Error | Percent Change | Notes |
|---|---|---|---|---|---|
| MechanicalVentilator-TidalVolume(mL) | EqualTo 650 | 658 | 1.30% | VT (measured) | |
| InspiratoryRespiratoryResistance(cmH2O_s/L) | LessThan Segment2 (33.3) [304] [308] | 10.1 | -69.8% | Rinsp | |
| ExpiratoryRespiratoryResistance(cmH2O_s/L) | LessThan Segment2 (50.6) [304] [308] | 10.1 | -80.1% | Rexp | |
| MechanicalVentilator-PeakInspiratoryPressure(cmH2O) | LessThan Segment2 (49.6) [304] [308] | 22.2 | -55.1% | PIP |
| Property Name | Engine Value |
|---|---|
| Patient-Height(in) | 69.0 |
| Patient-IdealBodyWeight(kg) | 70.7 |
| InspiratoryRespiratoryResistance(cmH2O_s/L) | 10.1 |
| ExpiratoryRespiratoryResistance(cmH2O_s/L) | 10.1 |
| RespiratoryCompliance(mL/cmH2O) | 59.1 |
| ClinicalPhysiologicDeadSpaceTidalVolumeRatio | 0.442 |
| ClinicalShuntFraction | 0.187 |
| MechanicalVentilator-TidalVolume(L) | 0.658 |
| BloodPH | 7.42 |
| Aorta-Oxygen-PartialPressure(mmHg) | 78.6 |
| Aorta-CarbonDioxide-PartialPressure(mmHg) | 39.6 |
| Aorta-Bicarbonate-Molarity(mEq/L) | 25.8 |
| OxygenSaturation | 0.963 |
| HorowitzIndex(mmHg) | 197 |
| IntrinsicPositiveEndExpiratoryPressure(cmH2O) | 0.180 |
| MechanicalVentilator-RespirationRate(1/min) | 18.0 |
| MechanicalVentilator-MeanAirwayPressure(cmH2O) | 7.33 |
| MechanicalVentilator-PeakInspiratoryPressure(cmH2O) | 22.2 |
| MechanicalVentilator-PlateauPressure(cmH2O) | 16.3 |
| HeartRate(1/min) | 96.1 |
| SystolicArterialPressure(mmHg) | 110 |
| DiastolicArterialPressure(mmHg) | 79.6 |
| MechanicalVentilator-TotalPulmonaryVentilation(L/min) | 11.8 |
| MechanicalVentilator-InspiratoryResistance(cmH2O_s/L) | 10.1 |
| MechanicalVentilator-ExpiratoryResistance(cmH2O_s/L) | 10.1 |
| MechanicalVentilator-StaticRespiratoryCompliance(mL/cmH2O) | 58.6 |
| MechanicalVentilator-DynamicRespiratoryCompliance(mL/cmH2O) | 38.1 |
| MechanicalVentilator-EndTidalCarbonDioxidePressure(mmHg) | 29.7 |
| MechanicalVentilator-EndTidalOxygenPressure(mmHg) | 272 |
| MechanicalVentilator-ExpiratoryTidalVolume(L) | 0.658 |
| MechanicalVentilator-InspiratoryExpiratoryRatio | 0.219 |
| MechanicalVentilator-InspiratoryTidalVolume(L) | 0.658 |
| MechanicalVentilator-PeakExpiratoryFlow(L/s) | 0.628 |
| MechanicalVentilator-LeakFraction | 0.00 |
| MechanicalVentilator-IntrinsicPositiveEndExpiratoryPressure(cmH2O) | 0.107 |
| MechanicalVentilator-ExtrinsicPositiveEndExpiratoryPressure(cmH2O) | 5.00 |
| MechanicalVentilator-TotalPositiveEndExpiratoryPressure(cmH2O) | 5.11 |
| PhysiologicDeadSpaceTidalVolumeRatio | 0.477 |
| PhysiologicShuntFraction | 0.191 |
| TotalRespiratoryModelInspiratoryResistance(cmH2O_s/L) | 10.1 |
| TotalRespiratoryModelExpiratoryResistance(cmH2O_s/L) | 10.1 |
| TotalRespiratoryModelCompliance(mL/cmH2O) | 66.2 |
| ExtrinsicPositiveEndExpiratoryPressure(cmH2O) | 5.00 |
| TotalPositiveEndExpiratoryPressure(cmH2O) | 5.18 |
| EndTidalCarbonDioxidePressure(mmHg) | 30.7 |
| PhysiologicDeadSpace(mL) | 236 |
| AlveolarArterialGradient(mmHg) | 189 |
| AlveolarDeadSpace(mL) | 94.9 |
| AnatomicDeadSpace(mL) | 141 |
| ChestWallCompliance(L/cmH2O) | 0.161 |
| FractionOfInspiredOxygen | 0.400 |
| LungCompliance(L/cmH2O) | 0.0972 |
| VentilationPerfusionRatio | 2.20 |
| HeartStrokeVolume(mL) | 58.5 |
| HeartEjectionFraction | 0.478 |
| BloodVolume(L) | 6.66 |
| MeanArterialPressure(mmHg) | 95.1 |
| PulsePressure(mmHg) | 29.9 |
| CardiacOutput(L/min) | 5.62 |
| CarbonDioxideSaturation | 0.0288 |
| RespiratoryExchangeRatio | 0.815 |
| SystemicVascularResistance(mmHg_s/mL) | 0.964 |
| OxygenConsumptionRate(mL/min) | 257 |
| CarbonDioxideProductionRate(mL/min) | 209 |
| Patient-AlveoliSurfaceArea(m^2) | 12.8 |
| Patient-ExpiratoryReserveVolume(L) | 0.876 |
| Patient-FunctionalResidualCapacity(L) | 1.97 |
| Patient-InspiratoryCapacity(L) | 3.13 |
| Patient-InspiratoryReserveVolume(L) | 2.59 |
| Patient-ResidualVolume(L) | 1.09 |
| Patient-TidalVolumeBaseline(L) | 0.540 |
| Patient-TotalLungCapacity(L) | 5.10 |
| Patient-VitalCapacity(L) | 4.00 |
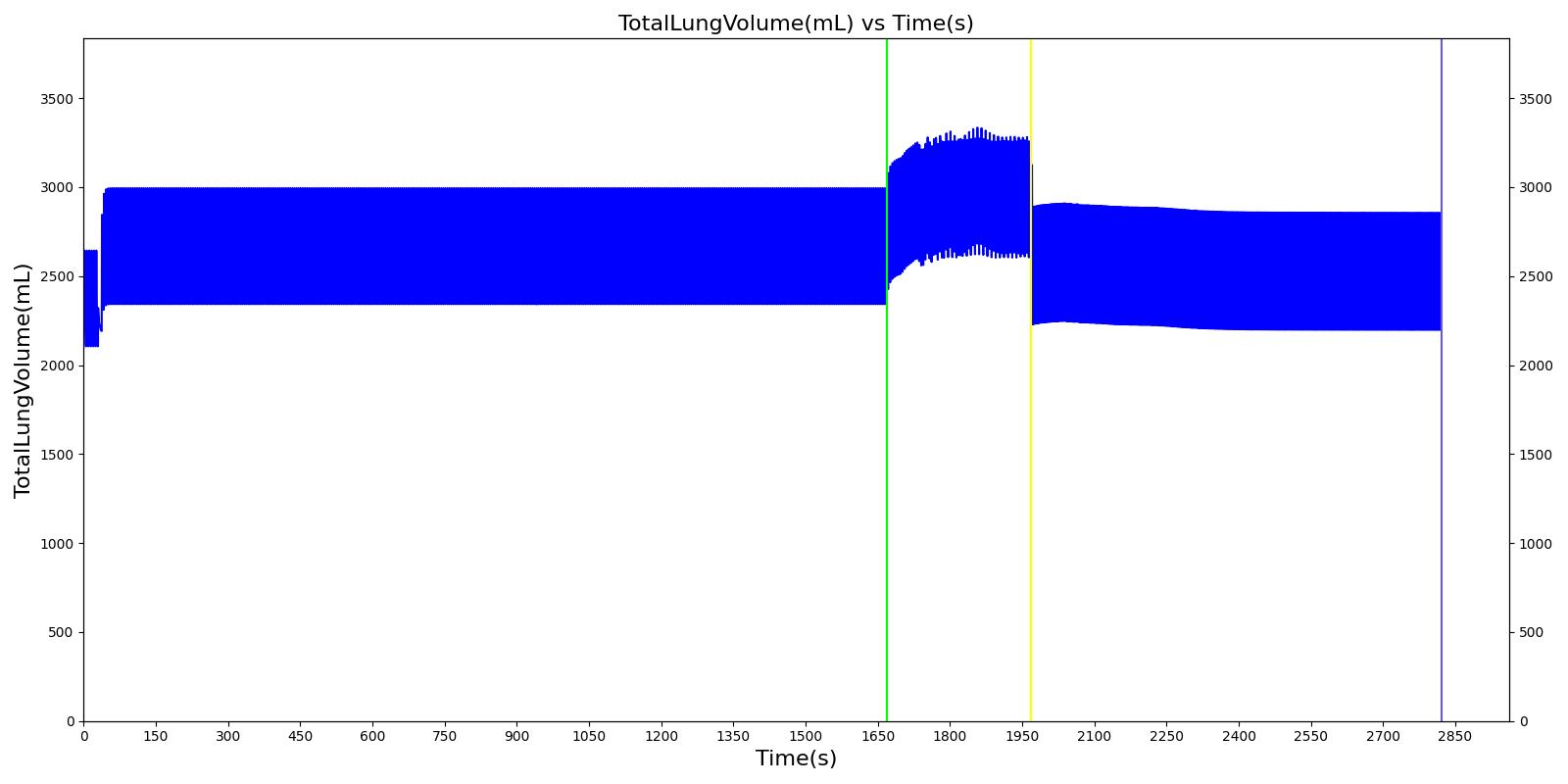
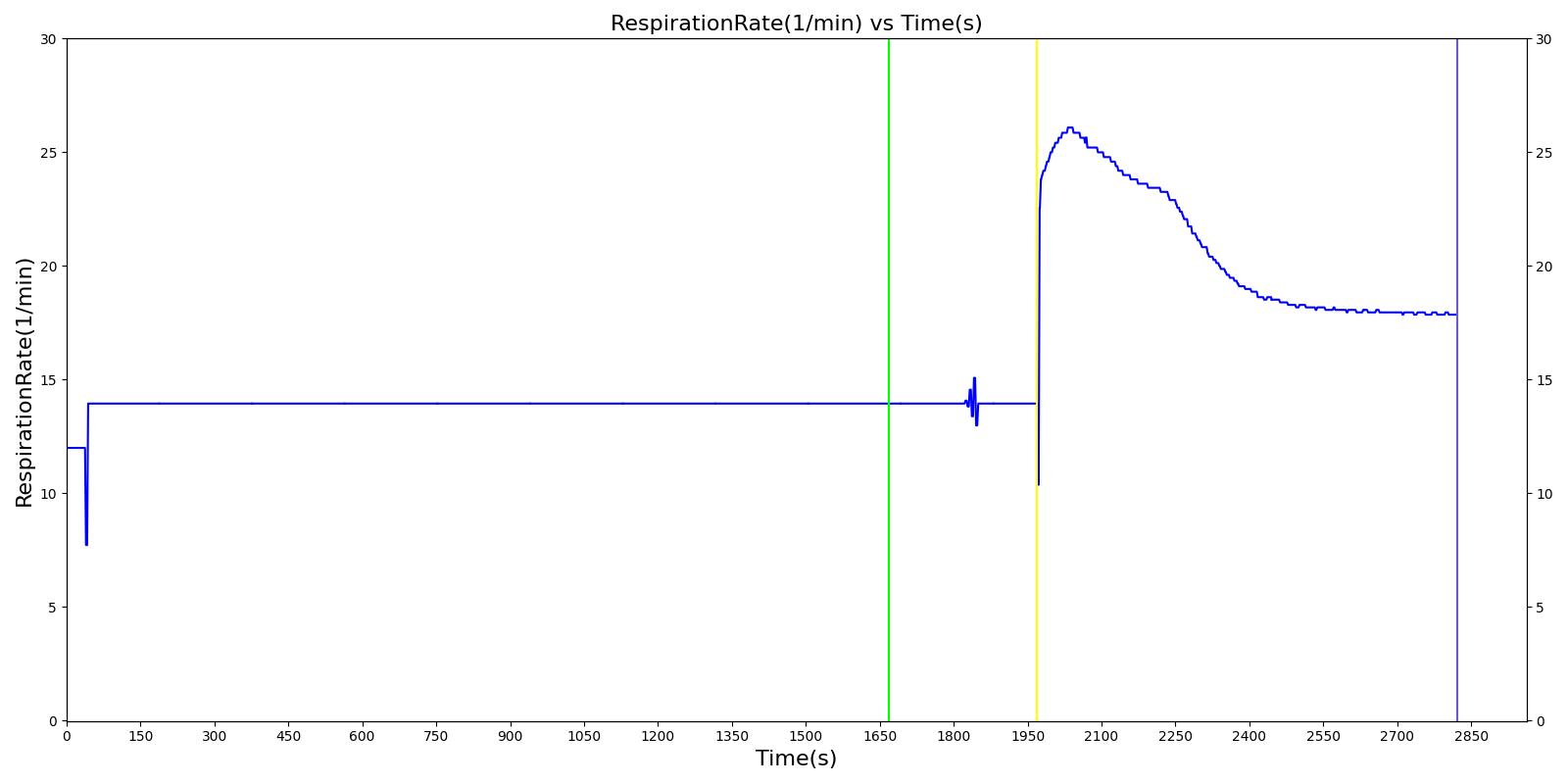
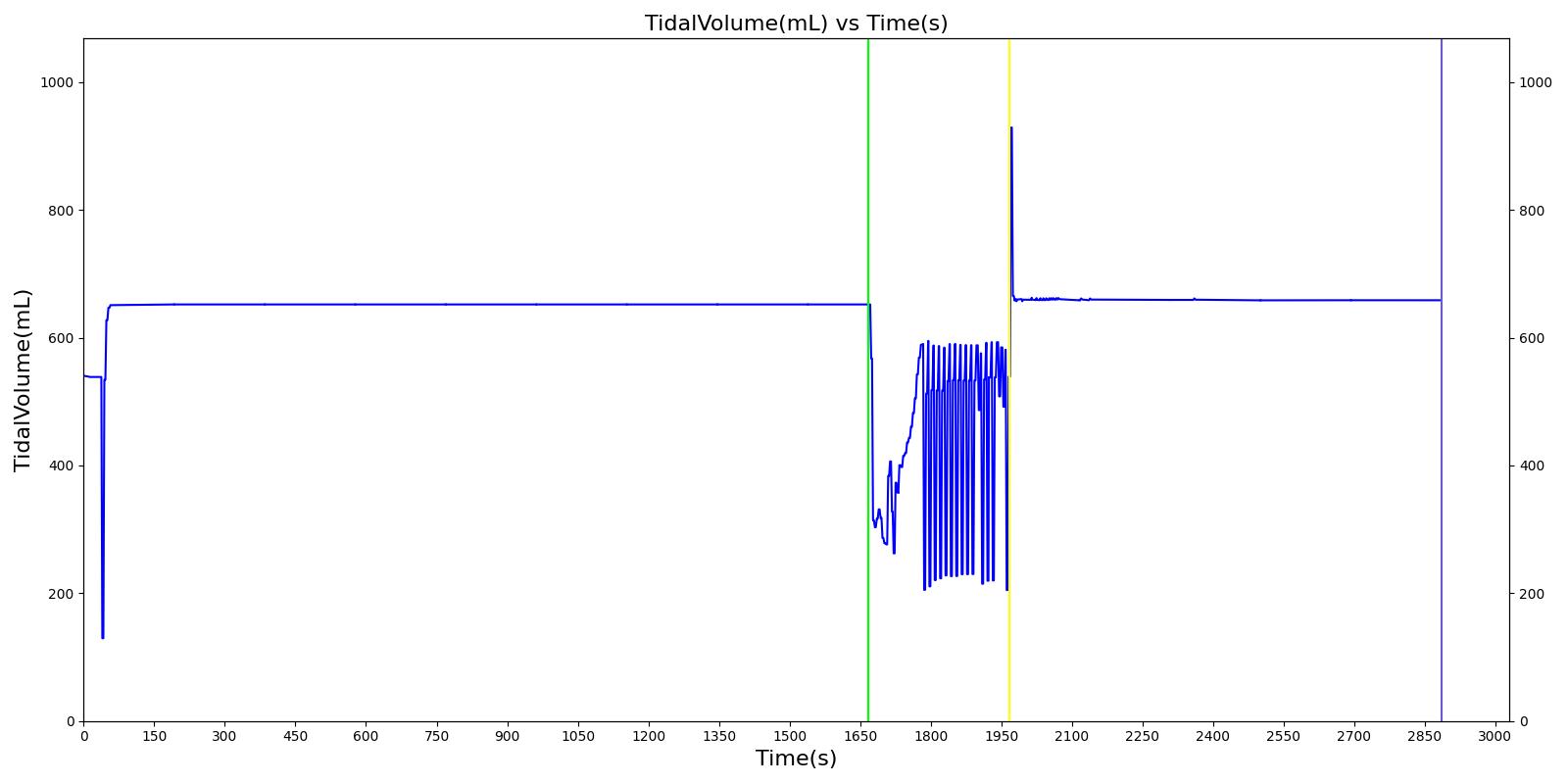
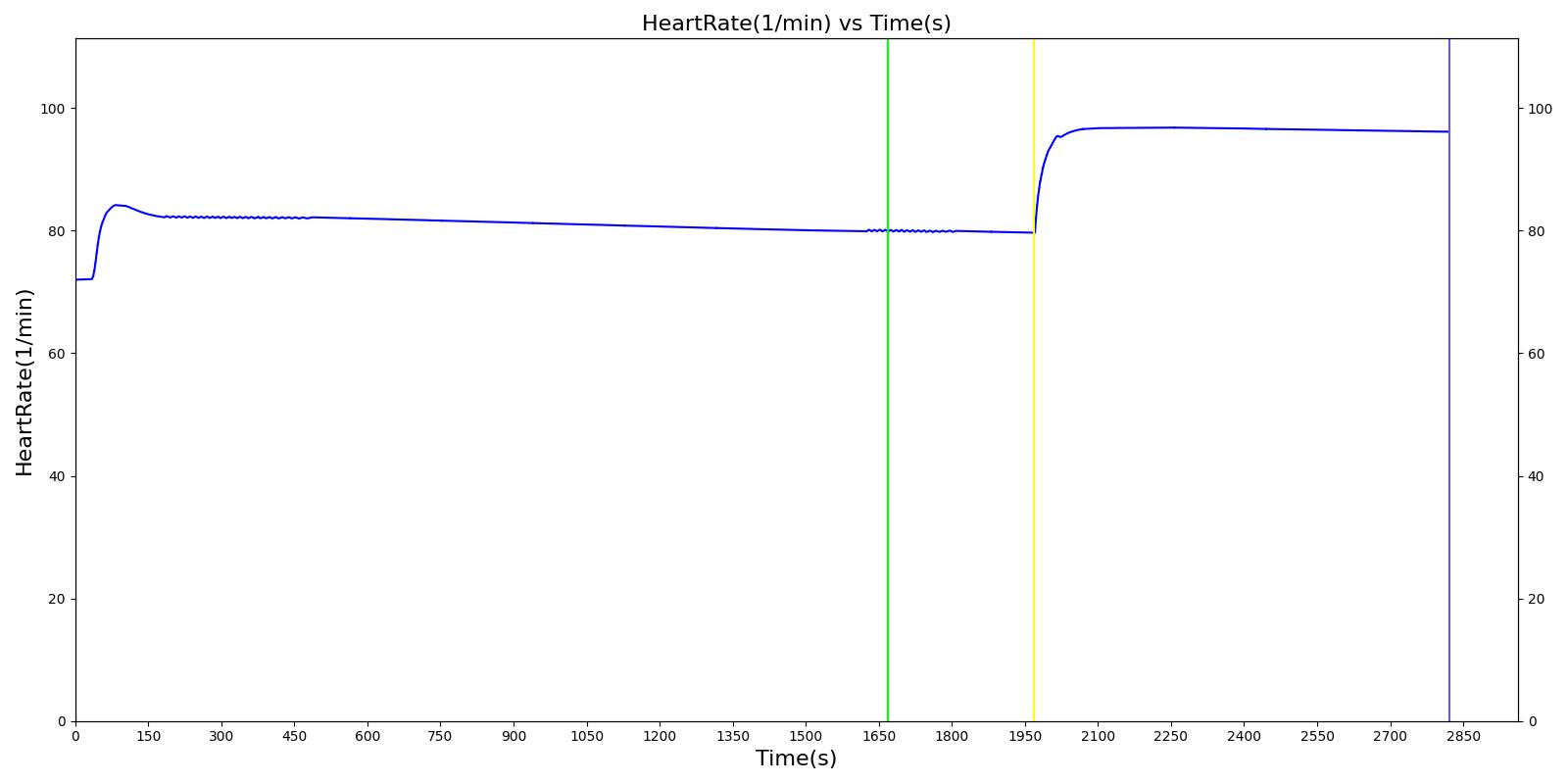
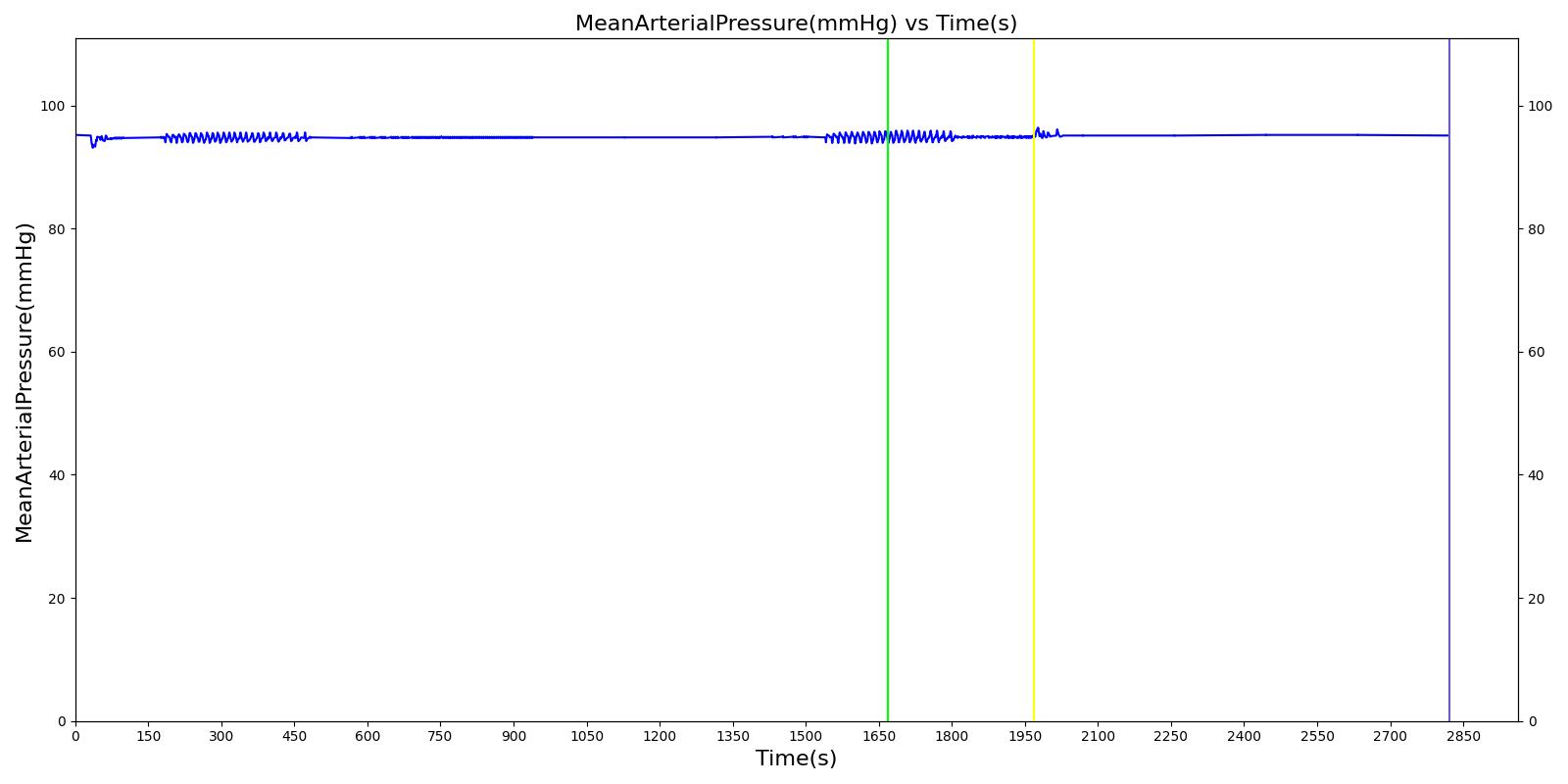
Scenario Output Plots
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
|